
This is a chapter from the book HYPOADRENOCORTICISM, copyrighted by
the Adrenal Metabolic Research Society of the Hypoglycemia Foundation,
Inc., 153 Pawling Avenue, Troy, New York, USA 12180. Upon the deaths of
Dr. Tintera, M.D. in 1969, and later his wife, the Tintera's heirs passed
all the collected papers of the Hypoglycemia Foundation, Inc. to the Hypoglycemia
Association, Inc. (HAI) This has been reproduced here with the permission
of HAI, Inc.
Vol. 1, No. 3, 1967
30 South Broadway
Yonkers, New York
The preparation of this paper has been aided by a grant from the Hypoglycemia
Foundation, P.O. Box 444, Scarsdale, New York.
A growing body of data lends strength to the conviction that schizophrenia
can no longer be considered a purely mental disease. Like alcoholism, schizophrenia
must be approached with the whole human organism in mind. This attitude
was proposed more than forty years ago by Meyer (1948). Our mission is
to coordinate and harmonize the "psyche" and the "soma"
through the principles of genetics, biochemistry, enzymology and especially
endocrinology. This can be no surprise even to the psychoanalyst. Over
two thousand years ago the ancients described the pineal gland as the seat
of the soul and in the seventeenth century Descartes agreed with them (Harvard,
1891). Freud himself was speaking of endocrinology when he said, "These
mental disturbances are open to therapeutic influence only when they can
be identified as secondary effects of some organic disease (Freud, 1943).
In recent years psychiatry has come to sense some limitation as a descriptive
science. Mere manipulation of the psyche left something to be desired.
Other disciplines were invoked. Surgery seemed too brutal. Convulsive therapy
was helpful as a last resort. The success of Hoffer (1957) with nicotinic
acid and diet is a promising step. The steady increase in mental hospital
population is the U.S. reversed itself abruptly in 1955 with the advent
of tranquilizers and antidepressants. By 1963 the mental hospital census
in the U.S. was 135,000 less than had been projected (Simpson, 1966). Although
they may have been spared hospitalization, the picture of 135,000 numbed
and somewhat toxic and sometimes addicted citizens is not entirely a satisfactory
one to contemplate.
Endocrine Aspects of Schizophrenia
Studies attempting to correlate psychotic states with adrenal function
are well known. (Bunny et al, 1965a; Bunny et al. 1965b; Suwa et al. 1962;
Curtis et al. 1960; Persky et al. 1959). Other investigators (Simon &
Gillies, 1954; Larsen, 1964) tried to associate mental aberration with
such physical attributes as bone and muscle measurements, fat distribution
and blood pressure, all of which may certainly carry endocrine connotations.
My firm belief in the vital importance of the endocrine system in pathological
mentation was sparked in the early forties when I first insisted on 3-4
hour glucose tolerance tests. The laboratories apologized for seemingly
incorrect readings although they had double-checked their techniques. What
mystified them was the low flat curves derived from disturbed early adolescents.
This laboratory procedure had been previously carried out only for patients
with physical findings presumptive of diabetes.
Dorland's definition of schizophrenia (Bleuler's Dementia Praecox) includes
the phrase, "often recognized during or shortly after adolescence",
and further, in reference to hebephrenia and catatonia, "coming on
soon after the onset of puberty."
These conditions might seem to arise or become aggravated at puberty,
but probing into the patient's past will frequently reveal indications
which were present at birth, and during the first year of life, and through
the pre-school and grammar school years. Each of these periods has its
own characteristic clinical picture. The picture becomes more marked at
pubescence and often causes school officials to complain of juvenile delinquency
or underachievement. A glucose tolerance test at any of these periods could
alert parents and physicians and could save innumerable hours and small
fortunes spent in looking into the child's psyche and home environment
for maladjustments of questionable significance in the emotional development
of the average child. The negativism, hyperactivity, and obstinate resentment
of discipline are absolute indications for at least the minimum laboratory
tests: urinalysis, complete blood count, P.B.I. determination and the 5-hour
glucose tolerance test. A glucose tolerance test can be performed in a
young child by the micro-method without undue trauma to the patient. As
a matter of fact, I have been urging that these four tests be routine for
all patients, even before a history or physical examination is undertaken.
In almost all discussions on drug addiction, alcoholism, and schizophrenia,
it is claimed that there is no definite constitutional type that falls
prey to these afflictions. Almost universally the statement is made that
all of these individuals are emotionally immature. It has been our goal
to persuade every physician whether he is oriented toward psychiatry, genetics
or physiology to recognize that one type of endocrine individual is involved
in the majority of these cases - the hypoadrenocortic. In most instances
he has an inborn error of metabolism, with failure in the production of
certain adrenal cortical hormones which initiate and control the interaction,
activation, and inhibition of certain enzymes. Alcohol dehydrogenase, for
example, has definitely been incriminated in the alcoholic and the barbiturate
addict. In the schizophrenic, time and again various peculiar metabolites
have been shown to be related to carbohydrate intake and reflect a breakdown
in the cycle in which the cerebral cortex activates the vegetative nervous
system which in turn stimulates the productions of catecholamines necessary
to mediate the hypothalamic-adrenohypophiseal-adrenocortical complex (Kaplan,
Inf. Comm.).
Hypoadrenocortical Syndrome
I first described the hypoadrenocortical syndrome in 1949 (Tintera &
Lovell, 1949) in connection with alcoholism and later, in 1955 (Tintera,
1955) summarized the typical findings in 200 selected cases. The chief
complaint were as follows:
Other findings according to organic systems are listed with their frequencies
in these papers. It is germane, however, to give here the chief physical
and laboratory findings.
We need not, and indeed should not, limit our consideration to the first
manifestation of schizophrenia in the pubescent child since even at birth
such ominous stigmata may be present as hyponatremia, hypoglycemia, hypomyotonia,
and hyperreflexia. The frequently premature offspring of parents who exhibit
allergies or other hypoadrenocortic indicia may have gastric symptoms such
as projectile vomiting or pylorospasm, often severe enough to be fatal.
Later we see the hyperactive preschool child and the underachiever in grade
school. His chief scholastic barrier is the inability to concentrate on
mathematics, and finally he fails algebra and/or geometry. Then there is
the negative adolescent with failure in development of secondary sex characteristics.
In typical sequence the colicky newborn develops diaper rash followed
by frank eczema. Later (after T. & A.), hay fever often arises which
may eventually lead to asthma (post-appendectomy) and finally schizophrenia
intervenes, at which time the allergies disappear. Incidentally, the post-appendectomy
asthma is an argument for the reticuloendothelial function of the appendix.
mesenteric adenitis mimics appendicitis; 85% of the removed appendices
are innocent.
Improvement in the schizophrenic is usually attended by a return of
asthma. We have demonstrated elsewhere that hypoadrenocorticism is the
basis of the allergic response (Blaine, 1965). Stress may activate the
hypothalamus-pituitary-adrenal axis to such an extent that sufficient steroids
are elaborated to control the allergy but at the same time the balance
is disturbed since ACTH is specific for glucocorticoids, but not for mineralocorticoids
and 17-ketosteroids to an equal degree. For this reason it is illogical
to prescribe individual steroids such as cortisone or cortisol without
regard to the synergistic and antagonistic hormonal relationship.
The endocrinologist is not mystified by the striking clinical improvement
in many psychiatric patients following electro-convulsive therapy. In addition
to interrupting the mental processes, this electrical insult to the organism
stimulates the adrenal cortex to pour out tremendous quantities of properly
proportioned corticosteroids (Graham & Cleghorn, 1951). This is beneficial
if the adrenal is able to respond but when the adrenal is already exhausted,
the result may be disappointing. E.S.T. has a definite place in the psychiatric
armamentarium provided the patient has been conditioned previously with
A.C.E. (adrenal cortex extract) but not with individual steroids which
only create imbalance among the 32 or more steroids involved. Employing
these principles of pre-treatment with A.C.E., Connason and Ryberg (1957)
obtained remarkable results, even in long-standing cases. In their series,
the milder foreign protein stimulus was used instead of electroshock.
Carbohydrate Metabolism
The only definitive gauge of impaired carbohydrate metabolism in the
schizophrenic and/or hypoadrenocortic is the five-hour glucose tolerance
test. In young individuals with hypoadrenocorticism or pituitary-adrenal
insufficiency, a low, flat curve is observed. This moderate hypoglycemia
induces a craving for carbohydrates, alcohol, or drugs which afford temporary
relief of symptoms such as nervousness and feelings of unreality. Hepatic
damage results from prolonged abuse of these agents. Fatty infiltration
follows glycogen depletion and the GTT curve then will be characterized
by a sudden initial rise to a high plateau followed by and abrupt drop,
technically reactive hypoglycemia. In the pituitary-adrenocortic with obesity
the rise reaches hyperglycemic levels and eventually declines to hypoglycemic
values. Without dietary indiscretions, the curve may remain flat until
the climacteric when again a further disturbance in the steroid balance
may arise as a result of gonadal failure. The adrenal produces 65% of the
male hormone in the man but only 15% of the female hormone in the woman
during the child-bearing years. The absolute shutdown of the gonads puts
a greater load on the already deficient adrenals and many acute episodes
are encountered at this age, especially in the female when the adrenals
are required to produce 100% of the estrogens.
Cortisone, or its derivatives, is not the answer to adrenal deficiency, as evidenced by a 13 year old girl who developed chronic nephrosis with marked edema. Hospitalized at one of our local university medical centers, she was given the generally approved dose of 60 mg. prednisone to which she did not respond. The dose was doubled to 120 mg., then to 240 and finally to 320 mg. per day, at which point this shy, unobtrusive child became a manic schizoid, destroying so much hospital

equipment she had to be restrained. The 4+ proteinuria persisted and
she, along with seven other children were considered failures on prednisone
and as a last resort, an untried experimental drug was proposed, whereupon
the protesting parents sought other advice.
When I first saw her, the urine boiled solid in the test tube. The day
after the initial dose of Eschatin the urine was absolutely clear. She
made a stormy but complete ambulatory recovery with A.C.E., diet, etc.
The GTT showed a sever diabetic curve. After recovery, a normal curve was
obtained, except for an exceptionally low fasting level, shown in Figure
1. What was the cause of schizophrenia in this case? Evidently, it was
a derangement of cerebral carbohydrate metabolism. During intensive A.C.E.
treatment, she was a good student, but now on maintenance does not concentrate
as well, failing most subjects, notably algebra, but she is alive.
Case Histories
The following case histories represent patient, who on the average had
previously been treated by 10 physicians and 2 psychiatrists. All demonstrated
moderate to severe emotional disturbances but no specific psychiatric diagnosis
is offered:
Case 1
Patient: T.H. First seen 6/5/62; Age 35; White female. Always
tired, born tired. Quite upset, cries for no reason. Difficulty in concentrating.
Good marks in school but had to study lying down. On and off thyroid (Proloid)
for 12 years. 2 children (never felt better than when pregnant. Put on
Dexedrine 1960, followed by hypoglycemia collapse Feb. 1960. On low-carbohydrate
diet for 4 months, then returned to regular diet. Same year spent 6 weeks
in psychiatric hospital for overdose of Librium where the diagnosis was
made of anxiety, neurocirculatory asthenia. Still on amphetamines. Saw
12 MDs in past year. Blood pressure has been 80/40. Craves sweets. Gets
rose fever and vasomotor rhinitis. Adores pickles.
PE.: Long index fingers, hypoadrenocortical teeth, positive Rogoff.
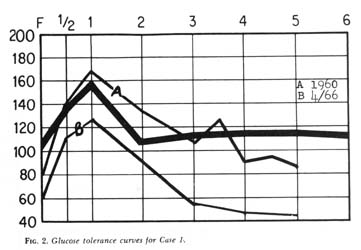
GTT: 1960: F-81, 1/2-136, 1-167, 2-133, 3-108, 3 1/2-123, 4-91,
4 1/2-95, 5-87. P.B.I.-11.8mcg%.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism (mild), autonomic
nervous system instability, orthostatic hypotension.
RX: AdrenalCortical Extract (A.C.E.) B6, B12, Theelin, Durabolin,
Belergal.
Course: Short periods of slight improvement through 7/28/62.
Patient not faithful to diet at first and continued to take tranquilizers,
but by 10/16/62 patient stated enthusiastically that she was functioning
one more as a human being. Discharged to family physician. Admitted to
hospital 8/1/64 with acute pyelitis, discharged 8/6/64. Admitted to hospital
1/29/65 with diagnosis of neurotic depression and conversion hysteria;
discharged 2/7/65. Admitted to hospital 4/13/66 in a hypoglycemia collapse,
at which time the glucose tolerance test was F-60, 1/2112, 1-127, 1-94,
3-56, 4-48, 5-46. Discharged 4/20/66. 11/23/66 - First consultation since
10/26/62. In and out of hospital four times. Had not been following diet.
Taking Eskatrol twice a day. Patient returned to hypoglycemic regimen.
11/28/66 - "felt like a zombie." Crying, depressed, can't concentrate.
12/13/66 - Patient is beginning to have periods of "feeling decent"
but can be thrown into panic by being forced to make a "decision."
Referred back again to family physician in a manageable state.
Patient: H.J. First seen 4/14/58; Age 21, White female. Fears
and anxiety (worse in crowds). Afraid to leave her house. Dizzy spells.
Saw psychiatrist 2-3 times a week for 3 years. Was "afraid" of
him. Had ambulatory shock treatment Oct. 1956 (3 electroshock -5 insulin).
Received increasing doses of Sodium amytal each visit - couldn't talk otherwise.
Less nervous driving car; short periods of employment. Took tranquilizers
- also Dexamyl. Perspires profusely; started to gain weight at 5 or 6.
Always a tom boy. Used depilatory last 3-4 years upper lip. chin, side
of face. Menstrual difficulties. No sex activities. Sighing respiration.
Trochanteric obesity at 12 or 13. Candy binges.
P.E.: Unremarkable, except for separation of upper incisors,
high palatal arch, mild hirsutism, long index fingers, 3-4 interspace tenderness,
positive Rogoff. Blood pressure 152/90. Ht. 5'5". Wt 135.
GTT: April 1958: F-90, 1/2-116, 1-86, 2-96, 3-80, 4-82.
Diagnosis: Mild hypopituitarism with secondary hypo-ovarianism
and hypoadrenocorticism.
RX: Diet, A.C.E. Benadryl. Theelin, B6, B12, Bellergal, Menagen,
Norlutin.
Course: Very slow improvement with gradula increase in activities outside the home. Employment status also improved. Many periods when symptoms returned - shaking, anxiety, panic, depression but by 11/2 years was married and moved to Wyoming. Works steadily and reports good general condition. Blood pressure normal. Death of 18-month old baby 1966 brought on period of "exhaustion". Determines own need for A.C.E. 5-10 cc per month. Leads comparatively extravertive life even withstanding the collapse of her dream to run dude ranch.
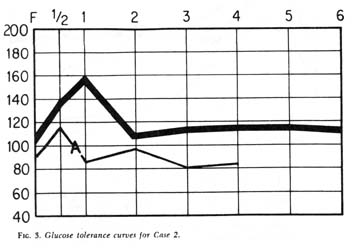
Patient: P.M. First seen 4/4/47; Age 32; White female. Depressed,
confused, irritable. Tired and too weak to stand. Migraine since age 17,
mild allergies. Fingers blanch with mild cold. Vague fears for self. Cries
often, "impossible to live with."
P.E.: Wt. 105, Ht. 65", blood pressure 136/82, positive
Rogoff (rt), dermographia.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism.
RX: Diet, A.C.E, Theelin, Gynergin, Hepthis, Cortate Pettets-DOCA,
Proloid, Presidon, Bellergal.
Course: Slow recidivous progress as activity increased. Much
improved with gain in weight. Patient not seen between Dec. 1956 and Jan
28, 1964, during which period she had required psychiatric hospitalization.
Now in a stormy menopause. Rogoff strongly positive. Slow progress again.
Course of shock treatments recommended 7/65. Tranquilizers and also Bellegral,
diet, A.C.E. (increased doses), Theelin, Valium, B6, B12, Norlutate, Menagen.
Within a month shopped. Now back at work and coping with unusual stress.
GTT: Jan 30, 1964: F-90, 1/2-137, 11/2-98, 2 1/2-78, 3 1/2-65, 4 1/2-79, 5 1/2-79
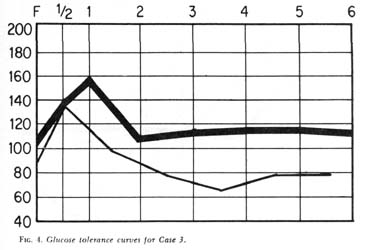
Patient: L.R. First seen 11/20/61 - Age 11.5 White female. Tired,
no energy, allergies. Can't concentrate, gets dizzy in math class. Colic
and projectile vomiting as an infant. Intense early family trauma. High
I.Q. Under psychiatric care. An emotionally disturbed child. Difficult
to manage.
P.E.: Wt. 77, Ht. 54", blood pressure 110/70, allergic conjunctivitis,
Vasomotor Rhinitis, mod. positive Rogoff, P.B.I 5.3mcg%
GTT: 11/1/61; F-110, 1/2-188, 1-183, 2-150, 3-112, 4-110, 5-102.
Diagnosis: Mod. hypoadrenocorticism, sexogen insufficiency, "emotional
disturbance."
RX: Diet, Lipo, A.C.E., Bellergal, API., Theelin, B6, B12, Will
need Proloid and progesterone.
Course: Steady dramatic improvement in school work, family relationships,
life interests and energy output. Discharged 10/64 and regular regimen
stopped and invented own diet. Menarche marked by irregularity at age 15.
Day of repeat Glucose Tolerance Test Oct. 1966 made a tentative attempt
to slash wrists and was hospitalized and given intensive endocrine therapy
with prompt favorable response. Outside school privileges as in-patient.
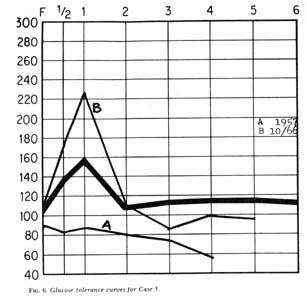
GTT: Sept. 1966: F-80, 1-224, 2-240, 3-191, 4-95, 5-42, 6-74.
Oct. 1966: F-80, 1/2-180, 1-230, 2-148, 3-130, 4-55, 5-67.
Patient: P.H. First seen 12/11/63; Age 37; White female. Depression,
agitation, tiredness since childhood. Life seemed bleak, lived from day
to day. Saw endocrinologist in 1961 for weight when she was told her Glucose
Tolerance Test was normal. (In 1957 it had been: F-88, 1/2-83, 1-87, 2-80,
3-71.7, 4-57). Has temper tantrums and screams at her 3 children. No interest
in sweets but likes pickles and pickle juice. Tried suicide by sleeping
pills 9 years ago. Intermittent treatment by psychiatrist. Has two siblings,
one in mental hospital, other has "nervous stomach"
P.E.: Wt 130, Ht. 5'1", blood pressure 120/62. Hyperactive
reflexes, mild girdle and lower trochanteric obesity, mild hirsutism, 4th
interspace tenderness. P.B.I. - 3 mcg%.
Diagnosis: Mild hypopituitarism, hypoadrenocorticism, hypo-ovarianism
and hypothyroidism.
RX: Diet, Bellergal, Menagen, Proloid, Theelin, A.C.E, B6, B12.
Later Durbolin, Norpramin.
Course: At first patient did not stay on diet and progress was
very slow. In 9 months felt very well and engaged in wide variety of activities.
Depression and fatigue followed series of serious stress situations but
is now enjoying life.
GTT: Oct 12, 1966: Afternoon GTT: F-105, 1/2-175, 1-206, 2-108, 3-88, 4-101, 5-95
Patient: K.B. First seen 6/23/59; Age 44; White female. Depression
at the smallest challenge; unable to handle decisions, cries for no reason;
so self-confidence; no interest in anyone or anything. Very attached to
mother. Hospitalized at 6 for overactive thyroid. Father died April 1948;
3 electroshock treatment at this time. Balked in panic twice at approaching
matrimony. Married Dec. 1948. Three children. Well during pregnancy, depressed
post-partum. Minimal sexual pleasure. Wanted whole family to live with
mother. Intolerable alcoholic husband.
P.E.: Wt 131, Ht. 65", blood pressure 152/85. Crowded lower
incisors, long index fingers, exaggerated reflexes, such trochanteric obesity,
4th interspace tenderness, P.B.I - 6.8 mcg%.
GTT: F-90, 1/2-139, 1 1/2-117, 2 1/2-71, 3 1/2-67, 4 1/2-59.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism, autonomic nervous
system instability
RX: Bellergal, Menagen, A.C.E. Theelin, Testosterone, Benadryl,
B6, B12, Durabolin, Deprol, Valium, Heparin and diet.
Course: Very slow undulant progress. Constant severe marital
aggravation. Took handful of Bellergal and Phenobarbital Feb. 1960. 4 electroshock
treatments April 1963. Very slow progress since then, not always diet-faithful.
Still "up and down" but excursions less wide, anxieties less
specific and able to work quite steadily. Still living under extreme uxorial
stress. Blood pressure drops with sense of well-being. Working steadily
with increased ambition. Highest Civil Service rating.
Patient: H.M. First seen 11/7/56; Age 23; White female. Nervous-crying
spells. Felt like an outcast at school. "Nervous breakdown" at
15. Thought her food was poisoned. Shock treatments. Closely attached to
mother. Eggs made her vomit. Married two years. Baby eight months old.
Cried all the time after baby was born. Didn't nurse it - afraid her breast
would sag. Afraid her mother would hurt the baby. Had shock treatment again.
Depressed. Cries. Can't sleep. Irrational with nembutal. Cowered in corner
at sight of sphygmomanometer. "I don't want any more shock treatments."
P.E. Wt. 106, Ht. 62", blood pressure 132/90. Swollen turbinates,
long right index finger, adrenal teeth. positive Rogoff, exaggerated reflexes.
GTT: F-100, 1/2 180, 1-155, 2-110, 3-95, 4-75.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism (mild)
RX: Diet, A.C.E., Benadryl, B6, B12, Theelin, Bellergal, Noludar.
Course: Dramatic improvement with first treatment. Uneventful normal
delivery 2/29/60. Felt well afterwards. Nursed the baby. Discharged. Felt
very well during next pregnancy but went into severe post-partum depression
6/27/61. Recovered at once with A.C.E. and is feeling very well.
Patient: D.H. First seen 3/13/61; Age 44; White female. Year
ago felt she was losing her mind and has not felt right since. Was afraid
she would strike people - would have to leave any social situation in panic;
couldn't look in a mirror, couldn't face strangers; couldn't take a bath;
afraid of harming children. Saw 3 psychiatrists - told cure would take
3 years. Taking Librium.
P.E. Wt. 133. Ht. 65", blood pressure 100/70. Crowding of
lower incisors, 4th interspace tenderness, liver enlarged and tender. P.B.
I. - 5.1 mcg%.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism.
RX: Librium, A.C.E., Theelin, B6, B12, Bellergal, Menagen.
Course: Progressed slowly, by 2 months was having more good days
than bad. Good periods lengthened slowly. Specific phobias lessened greatly.
Patient now performing quite normally with occasional bouts of fearfulness
under severe stress situations, as when unwed daughter became pregnant.
GTT: 2/2/61; F-92, 1/2-135, 1 1/2-94, 2 1/2-87, 3 1/2-70, 4 1/2-84.
Patient: T.L. First seen 5/10/66; Age 31; White female. Nervous
breakdown, disturbed anxiety, depression for one year. (Diagnosed by psychiatrist
- schizophrenia with paranoid tendencies.) Tofranil made her worst. Also
had hepatitis. Thinks often of suicide.
P.E.: Weight 120, Ht. 64", blood pressure 110/70, conjunctivitis,
spots of pigmentation on neck, long index fingers, Rogoff tenderness, exaggerated
reflexes. P.B.I. - 4.8 mcg%
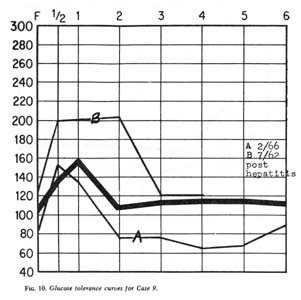
GTT: 2/6/66; F-88, 1/2-153, 1-135, 2-78, 3-78, 4-65, 5-68, 6-85.
7/62 post-hepatitis: F-124, 1/2-200, 2-202, 3-120, 4-120. (hepatic curve)
Diagnosis: Hypoadrenocorticism
RX: A.C.E., B6, B12, Estrogens.
Course: Gradual definite improvement in mood. Increased energy
and complete absence of all original complaints as of 12/66.
Patient: C.S. First seen 9/25/62; Age 42; White female. Referred
with diagnosis of hypoglycemia. Nervous, doesn't sleep. Deep sense of inadequacy,
afraid of losing her job. (even when employer promotes her and pays her
more). No energy. Ten years ago had a "nervous breakdown" described
as paranoid schizophrenia. Recent consulting psychiatrist thinks psychotic
exacerbation possible. Gets rose fever. Already on hypoglycemia diet and
tranquilizers.
P.E. Wt.136, Ht. 63", blood pressure 110/70, P.B.I. - 6.2
mcg%. Swollen tubinates, sl. crowding lower incisors, long index fingers,
moderate trochanteric obesity.
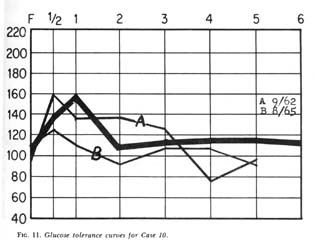
GTT: F-96; 1/2-159, 1-135, 2-136, 3-125, 4-77, 5-97.
Diagnosis: Hypoadrenocorticism, Mild hypo-ovarianism.
RX: Decreased tranquilizers, A.C.E., Menagen, Bellergal, B6, B12, Durabolin, Theelin.
Course: General improvement was rapid. Emotional state and energy
output goo. Fear of losing job and sense of inadequacy in that respect
kept returning in various degrees. Had 7 electroshock treatments in July
1963. The "job fixation" has been reduced and other wise the
patient feels very well.
GTT: 8/3/65; F-111, 1/2-125, 1-108, 2-92, 3-108, 4-108, 5-92.
Patient: S.B. First seen 10/22/58; Age 33; White female. Eczema
at five. Asthma since six-severest with first pregnancy. Recently every
morning. Always controlled with Tedral and Phenobrab. Food allergies during
emotional upheavals. Depressed, nervous, snaps at people. Pain in her chin
since adolescence - worse with nervous spells. Chews her lips until they
are sore. Had a short "nervous breakdown" - screaming nude in
the street, thought husband wanted to kill her. Had psychotherapy but no
shock treatment. Has no feeling for her 10 year old son "effeminate."
P.E.: Wt. 133, Ht. 65", blood pressure 118/72. Allergic
rhinitis, adrenocortical teeth, high narrow palatial arch, 4th interspace
tenderness, pos. Rogoff on rt., exaggerated reflexes. Mod. trochanteric
obesity.
Diagnosis: Hypoadrenocorticism, hypo-ovarianism.
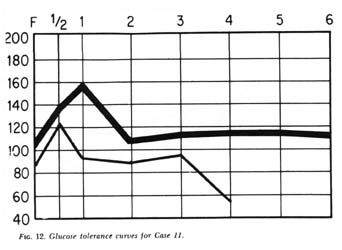
GTT: F-89, 1/2 -123, 1-92, 3-98, 4-54.
RX: Diet, A.C.E. Benadryl, Bellergal, Menagen, B6, Theelin, Norlutin,
Diuril, Aldactone.
Course: Rapid improvement until wheezing attacks became rare.
Two or three acute hypoglycemic episodes with severe schizoid manifestation
associated with diet lapses. Dramatic instantaneous recovery during intravenous
injections of Eschatin by family physician. Great improvement in mood.
Activities extended to include water skiing and travel to Europe. Has gone
through hay fever seasons without any asthma.
Case 12
Patient: L.C. First seen 6/20/62; Age 11; White female. Bright
fidgety and nervous, inattentive in school. Gaining weight. Steals money
and useless trinkets, mostly from family. Impossible to reason with. Was
thumb-sucker when young, also some colic and projectile vomiting as an
infant.
P.E.: Wt. 97, Ht. 60", blood pressure 100/50, P.B.I. 4.8
mcg%. Swollen turbinates, crowded lower incisors, long right index finger,
sluggish reflexes.
Diagnosis: Inborn error in metabolism, hypoadrenocorticism (mild),
hypothyroidism (mild).
RX: Diet, Intramuscular A.C.E. (in oil), Proloid, Bellergal,
B12, Theelin in small doses.
Course: Gradual improvement in personality and school work. Went
from failing student to honor student. At age 17 however, indulged in sexual
reveries almost hallucinatory in degree. Reported imaginary sexual debauches
as fact. This has since cleared up.
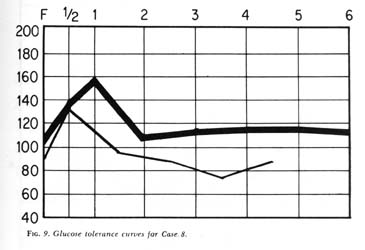
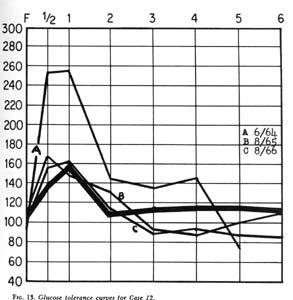
GTT: 8/5/65; F-90, 1/2-168, 1-150, 2-127, 3-91, 4-85, 5-100, 6-109
8/30/66; F-90, 1/2-155, 1-160, 2-105, 3-90, 4-90, 5-87, 6-85.
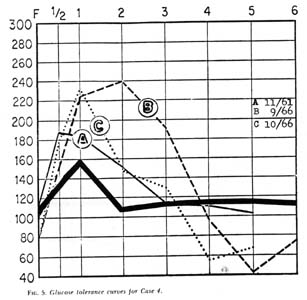
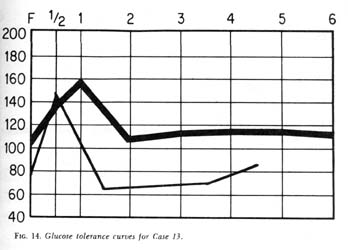
Patient: C.M. First seen 5/11/60; Age 66; White female. Repeated
periods profound depression starting with menopause in 1943. Two courses
of electroshocks - last one in 1954. Now on Nardil. Referred by psychiatrist
as a "hopeless case."
P.E.: Wt. 150, Ht. 64", blood pressure 134/70. Crowded lower
incisors, long right index finger. Some pigmented moles. Positive Rogoff.
Some pitting edema of ankles. Strongly exaggerated reflexes, marked Kraurosis
vulvae.
GTT: 4/28/60: F-81, 1/2-143, 1 1/2-67, 2 1/2 -67, 3 1/2-70, 4
1/2-84.
Diagnosis: Hypoadrenocorticism, post-menopausal syndrome, autonomic
nervous system instability, allergic diathesis.
RX: Diet, A.C.E.< Menagen, Bellergal, Theelin, Benadryl, B6,
B12. Reduce Nardil. Librium later prescribed.
Course: Steady progress with fewer more shallow periods of depression
at greater intervals until at the present she leads a very full life with
much activity in the arts, education and travel. Endures stress extremely
well. She has recently been awarded a high public honor.
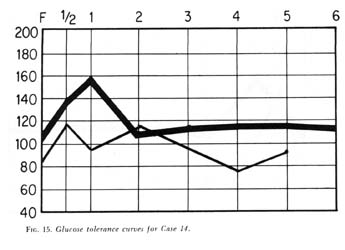
Patient: V.C. First seen 4/10/65; Age 17; White female. Tired
and depressed. Frequent headaches, no interest in anything. Gets dizzy
dressing, has to sit on bed. Cries for no reason. Can't concentrate. Panicked
at college boards. Feels something terrible is going to happen to her.
Hay fever history, also enuresis.
P.E.: Wt. 126, Ht. 64", blood pressure 118/74. Marked vasomotor
rhinitis, some crowding of lower incisors, some hair upper lip, long index
fingers, 4th interspace tenderness, positive Rogoff, overactive reflexes.
P.B.I. - 6.2 mcg% (taking 1 gr. thyroid daily).
GTT: F-87, 1/2 - 115, 1-96, 2-115, 3-95, 4-78, 5-95.
Diagnosis: Moderate hypoadrenocorticism. Slight estrogen deficiency.
RX: Diet, A.C.E., Progesterone, Theelin, B6, B12, Norpramin,
DOCA, Proloid, Librium.
Course: Stormy slow progress with candy binges and spells of
depression, withdrawal, and banging head on floor. Attitude at times has
approached catatonia. Has been able to work as a salesgirl and is better
able to manage her depressions. Wants to go to college and has been admitted.
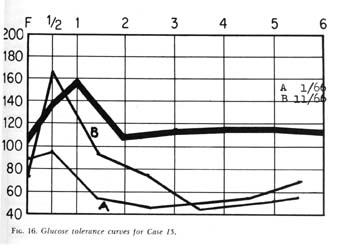
Patient: H.W. First seen 1/19/66; Age 43; White male. Asthma,
hay fever, "skin condition", rhinitis, started 22 years ago.
Called "shrimp" as a boy. Sense of nervous compulsion. Colchicine
etc. for gout one year ago. Lost sense of taste several years ago. Craves
sweets. Haunted by continuous sense of anxiety.
P.E.: Wt 137, Ht. 68", blood pressure 110/84. P.B.I. -8.7
mcg%. T3 1.09. Long index fingers, gouty deformation of the hands, crowded
lower incisors, skin lesions back scalp and left sternum, engorged thyroid,
pigmented nevae, Rogoff sign mod. pos., exaggerated reflexes.
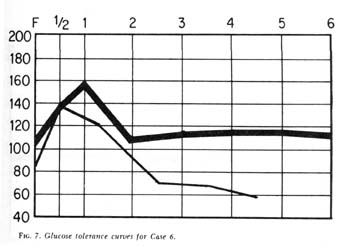
GTT: 1/8/66: F-84, 1/2-98, 1 1/2-56, 2 1/2-46, 3 1/2-50, 4 1/2-53, 5 1/2-70.
PM Test: 11/4/66: F-73, 1/2-165, 1 1/2-96, 2 1/2-75, 3 1/2-44, 4 1/2-48,
5 1/2-56
Diagnosis: Marked adrenal insufficiency, autonomic nervous system
instability, severe seborrheic dermatitis of scalp and torso, gouty arthritis.
RX: Diet A.C.E., Bellergal Spacetabs, Bellergal, B6, B12, Vitamin
C, Testosterone, DOCA.
Course: Marked improvement in mental outlook, upsurge in ambition
and energy output. Got very much improved. Rare headaches. Sense of smell
returned. Asthma disappeared. Gave up smoking without noticing it. Seborrhea
cleared completely and only pigmented areas remain on chest and lumbar
area.
The aspect of the patient's present gratifying sense of general well-being
is most important to him is at the same time the most interesting to the
physician. For twenty years the patient has been operating successfully,
writing books, mastering difficult engineering techniques and carrying
a heavy teaching load. Now to his amazement the realization comes that
throughout his adult life he has been driving himself mercilessly in the
face of terrifying anxieties and discomfort. His present life is such a
new and different experience that he doesn't see how he ever survived.
Patient: L.E. First seen 12/9/64; Age 44; White female. Referred
- already under treatment for hypoglycemia. Shaking and nauseated. Wakes
at 3 AM with pain and severe palpitation. Two courses of electroshocks
in July 1964. First one helped, second one made her feel worse - couldn't
stand them. Thorazine makes her scream, kick, and pound. At various times
has been dizzy, weak, nauseated. She has had shaking of the arms and legs,
quivering inside. Crying, worried, depressed. Felt like screaming or dying.
Masturbated as often as 30 times in one day. Treated in 1964 for hyperglycemia
with orinase. Normal blood curve returned. Now "cries all the time,
can't stand people or radio." Can't drive a car now - use to relax
her. Can't take Bellergal. Inactive pulmonary tuberculosis.
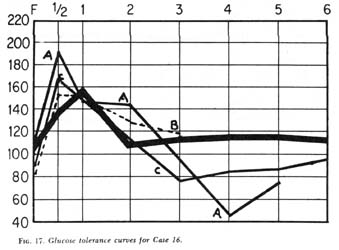
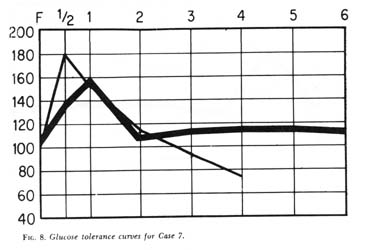
GTT: 1962: F-115, 1/2-189, 1-147, 2-147, 3-94, 4-42, 5-74.
11/21/66: f-92, 1/2-168, 1-144, 2-112, 3-76, 4-84, 5-84, 6-92.
Aug. 1964: F-81, 1/2-158, 1-153, 2-129, 3-119.
P.E.: Wt. 136, Ht. 66", blood pressure 128/82 T-3 1.06 Crowded
lower incisors, long index fingers, 4th interspace tenderness, positive
Rogoff sign. Progesterone obesity.
Diagnosis: Marked hypoadrenocorticism, hypo-ovarianism (estrogen
and progesterone deficiency), marked vagal involvement (damaged by TBC
chest surgery).
RX: Diet, A.C.E., Theelin, Durabolin, B6, B12, Belladonna, Quindine,
Menagen, Norlutin, Quinaglute, Norpramin, Valium, Calcium Benadryl, Ascorbic
Acid.
Course: Signs and symptoms dropped away one by one. Shaking and
quivering ceased. Mood improved and crying stopped. Masturbation ceased.
Took up automobile driving again. Fondness for music returned. Took part
in an amateur entertainment and was offered some professional contracts.
This after being certified for long-term complete disability.
More than twenty years ago Selye (1946), Long (1940), and Britton (1932)
reported animal experimentation with A.C.E. that convinced the writer that
the hypoglycemia which follows glucose intake is caused primarily by failure
of the adrenocorticosteroids to inhibit insulin activity and influence
the rate of insulin catabolism (Ingle, 1944). This hypothesis has been
corroborated recently by experiments which indicate that insulin induced
hypoglycemia stimulates the productions of glucosteroids by the adrenal
cortex (Plager & Matsui, 1966). The insulin level reached is not high
enough to justify the term hyperinsulinism. It was concluded that the activation
of the hypothalamic-pituitary-adrenal system is not so much a function
of the fall in blood glucose below an absolute level as it is of the rate
of glucose fall. This reaction is modified by the initial level of blood
glucose. The GTT is therefore a delicate indicator of the ability of the
C.N.S. and especially of the hypothalamus to activate the neural and humoral
pathways to the pituitary. In pituitary failure there is no response to
insulin administration even though the rate of blood glucose could be sufficient
to produce adrenal response in cases with intact pituitaries.
Within the past year. Plager and Matsui (1966) have demonstrated in
vitro what has been postulated in vivo that there is a graded
antagonism between various dose levels of cortisol and insulin. Unfortunately,
current animal experimentation does not deal with the whole extract since
cortisol is generally presumed to be the principal ingredient in such a
preparation and therefore there is a dearth of recent laboratory data on
the obvious synergistic-plus-antagonistic activity of the whole extract.
However, this writer has reported repeatedly and at some length on the
highly beneficial results obtained in 25 years of clinical use of A.C.E.
(Tintera & Lovell, 1949; Tintera, 1955; Tintera 1966).
As we know, the human organism operates for the most part on glucose
which must be supplied by the blood at the appropriate concentration. It
is understood that the adrenal cortex, through the operation of the glucocorticoids
plays a major role in regulating this concentration but there are many
intricate systems involved in carbohydrate metabolism; particularly enzyme
systems of the "Kreb's cycle". These operate in all tissues at
the cellular level, especially in the muscles and the liver. The enzymes
of the liver necessary for glycogenolysis and gluconeogenesis have been
identified. Alcohol dehydrogenase and other enzymes implicated in psychopathological
conditions have been less thoroughly investigated although they play a
role in alcoholism and drug addiction.
The other organs participating in carbohydrate metabolism have received
too little attention. For instance, the prostate is responsible for the
metabolism of fructose. Chronic benign prostatic hyperplasia is a frequent
concomitant of schizophrenia and is not necessarily an erotic manifestation.
Roberts (1966) has pointed out that the intactness of the testis, the pituitary
and the adrenal is necessary for accelerated prostatic growth. Prostatic
hyperplasia can be exaggerated by the increased elaboration of growth hormone,
adrenocortical steroids and pituitary prolactin or interstitial-cell stimulating
hormone under the repeated stimulus of recurrent hypoglycemia. Androgens
exert a diabetogenic effect as do these counter-insulin responses. The
high zinc, fructose, and enzyme content of the prostate favors the production
of insulin and thus may induce hypoglycemia.
The kidney contributes perhaps 15-20% of the inflow of glucose as calculated
from arteriovenous differences and renal blood flow (Cahill, 1964). This
will be discussed below:
Treatment
The importance of diet in the treatment of hypoglycemia (Physician's
Guidelines, 1966) cannot be overemphasized. There must be strict elimination
of all rapidly absorbable carbohydrates. This forestalls the sudden rise
and subsequent fall in blood sugar levels. The heightened protein intake
is beneficial in its own right since individual amino acids evoke rises
in circulating glucose (Fagans, Unp-Lecture).
Vitamin intake should be monitored to facilitate proper liver (B6) and
adrenal function (B1, 2, 6, 12, & C). Ascorbic acid is particularly
important since adrenal requirements for this vitamin are greatly increased
by stress.
In most instances if tranquilizing agents have been prescribed they
may be reduced in dosage when agents influencing the autonomic or vegetative
nervous system are prescribed. The A.N.S. undoubtedly plays a major part
in converting emotional stimuli into symptoms. In order to minimize the
role of emotions in the production of functional symptoms in patients with
adrenal insufficiency, it has been found advisable to prescribe a combination
(Bellergal) of 1-hyoscyamine, ergotamine tartrate and phenobarbital. Large
doses of this preparation are not required because of a synergistic action
with adrenal cortical extract. Patients are generally started on three
tablets a day, one on arising, one at about two o'clock in the afternoon
before the expected fall in blood sugar, and then one between dinner and
retiring. Portis has demonstrated that paralysis of the right vagus nerve
with large doses of atropine will prevent the inevitable fall in blood
sugar (Portis, 1950; Portis & Zitman, 1943). After approximately one
to two months the Bellergal may be reduced to two tablets daily. This dosage
has been continued for as long as six years. this autonomic system-oriented
preparation helps reduce the intensity of emotional stimuli, thus acting
to prevent the development of functional disturbances. In my estimation
this is one of the most valuable drugs available to the physician.
In mild cases at least 10 cc. of A.C.E. are given intravenously (or
if practical, intramuscularly) at least once a week for one to two months.
In severe, acute cases 10 cc injections may be required as often as every
four hours for the first 24 hours; the q. 8 hr. until it seems clinically
possible to give daily injections which may be continued for 1-2 weeks.
After that, weekly injections may be given indefinitely until the interval
between treatments may be progressively increased to two weeks, three weeks,
etc. Pyridoxine, 1.0 cc (50 mg.) is added to the solution of A.C.E. at
least once a week because of the role of this vitamin in the enzyme systems
involved in regulating carbohydrate metabolism. Also for its synergistic
and antihistaminic sedative effect, the optional addition of 1 to 5 cc
of Benadryl hydrochloride solution to the intravenous infusion is sometimes
desirable.
The use of A.C.E., especially if given intravenously, produces a temporary
feedback inhibiting the pituitary from whiplashing an already exhausted
adrenal and gives a refractory period of about fours hours to the cells
in the zona fasiculata and zona reticularis. At the same time, the level
of circulating glucosteroids is elevated so that restorative processes
can take place in the liver. With stabilization of the blood sugar, the
over-stimulated pancreas is also given a period of respite. However, if
cortisone or one of its derivatives is given in place of A.C.E., this steroid
would have to be given in divided doses of at least 100 mg. or its equivalent,
which would completely inhibit the pituitary and thus the secretion of
glucosteroids by the cells of the zona fasiculata and if given over an
extended period, atrophy of these cells would occur and further adrenal
insufficiency would result. In fact, continued use of individual glucosteroids
will invariably increase the level of blood glucose so that diabetic levels
develop.
ACTH is also contraindicated in these patients since it would tend to
whip the already exhausted adrenal cortex, producing hypertrophy and possibly
hyperplasia of the cells of the zona fasciculata, but with little beneficial
effect upon the mineralosteroid-producing cells in the zona glomerulosa
save for further slight water retention.
For males - Testosterone proprionate 50 mg. I.M. once a week initially
and methyl testosterone (Oreton) 19 mg. b.i.d. -- p.c. daily buccal administration
- no more than 2 gm. over a 3 month period. To help restore nitrogen balance
and further reduce demands on the adrenals - Adroyd or Maxiboten may be
used. When intervals have been increased to one month, 1cc Decadurabolin
may suffice to maintain a positive nitrogen balance.
For females - after negative Pap smear and culpocytology - Theelin or
conjugated 5 mg. (50,000 i.u.) weekly injections, and natural estrogens
(Menagen or Premarin) orally daily (during child-bearing years from the
3rd through the 26th day of menstrual cycle). If there is a history of
fibroids or dysmenorrhea, progesterone may be beneficial in addition to
the estrogen (from the 12th through the 26th day of the menstrual cycle).
Some comment is indicated on the various medicaments mentioned in the
foregoing resumes. There seems to be some misunderstanding as to the use
of the whole natural adrenal cortical extract (A.C.E.). It is uniquely
valuable and safe (Mod. Drug Encyl., 1965). In addition, it is effective
for long term use and in many cases should replace the corticosteroids.
To our personal knowledge more than 50,000 individual doses (10 cc or more)
have been administered over 20 years with no report of undesired side effects
and with consistent reports of beneficial results, often dramatic. In extreme
cases or in conjunction with surgery, dosage may be as high as 200 cc so
long as salt intake is maintained. Lipo Adrenal Cortex is also available
for intramuscular use. One cc of this preparation is equal to 10 cc of
the aqueous extract.
Bellergal has been dealt with elsewhere at some length. Other drugs
are of special interest mainly because of unwanted or toxic side effects.
Large doses of chlorpromazine for instance over a long period will substantially
reduce the secretion of ACTH (Bass, 1965). Hepatic toxicity (jaundice)
(Fajans Unpl. Lecture) has been reported from isocarboxazid (Marplan),
phenelzine sulfate (Nardil), imapramine hydrochloride (Tofranil), and desipramine
hydrochloride (Norpramin, Pertofrane). Many reports have dealt with hypertensive
reactions resulting from the ingestion of cheese while taking any of the
monoamine oxidase inhibitors: Marplan, Nardil, nialamide (Niamid), tranylcypromide
(Parnate). The antidepressants should not be prescribed for patients with
epilepsy or impaired kidney function.
The minor tranquilizers, chlordiazepoxide (Librium), chlormezanone (Trancopal),
diazepam (Valium), and meprobmate (Miltown-Equanil, etc.) can cause less
severe but definite adverse hepatic and renal effects.
Since hypoadrenocorticism is characterized by hyponatremia and hypo-kalemia,
these side-effects must be kept in mind. Hyponatremia, a factor in the
"Inappropriate Antidiuretic Hormone Syndrome," causes headache,
disorientation, somnolence and other cerebral symptoms. Severe headaches
often accompany the alkalosis associated with hypokalemia. Pending electrolyte
adjustment these can be relieved by glutamic acid-hydrochloride in doses
large enough to acidify the urine. As we have seen, the kidney in man contributes
perhaps 15-20% of the inflow of glucose. Any agent which would depress
renal glycogenesis could theoretically result in symptomatic hypoglycemia
within an hour (Roberts, 1966). It is well therefore when prescribing any
of these drugs to be alert to possible toxicity for the liver, kidney,
and cerebrum.
When the hypoglycemia of hypoadrenocorticism associated with schizophrenia
has been recognized, the administration of A.C.E. and the institution of
appropriate diet and supportive medication will fill only the immediate
needs of the patient. At this point the talents of the psychiatrist are
vital. His approach may be altered somewhat but the guidance of the physician-psychiatrist
is of prime importance in the restoration and maintenance of the desired
homeostatic state, the reflection of the nutritional, hormonal, and nervous
function of the body. The psychiatrist must lead these physiologically
inadequate and often emotionally immature individuals to full maturation
by regulating their activities and guiding them in their adjustment to
society and in the acceptance of their limitations and in the avoidance
of stressful situation.
Summary
The individual with constitutionally inadequate carbohydrate metabolism
has been described as the potential and genetic candidate for schizophrenia.
Recognition is most easily made through correlation of symptoms and
readings during a five-hour glucose tolerance test, and the interpretation
of the curve (Tintera, 1966).
Although many mentally or emotionally disturbed individuals seem to
make adjustment through diet alone, the underlying hypoadrenocorticism
must be treated. The regime of choice includes A.C.E., ancillary hormonal
therapy, supportive medication, and personal counseling.
References
Bass, Allan D. Drugs Affecting adrenocortical function. Postgraduate Medicine, 1965, 37, 82.
Blaine, T.R. Goodbye allergies. New York; Citadel Press, 1965.
Britton, S.W. & Silvette, H. The effects of cortico-adrenal extract on carbohydrate metabolism in normal animals. American Journal of Physiology, 1932, 100, 693-700.
Bunney, W.E., Jr., Mason, J.W., Roatch, J.F., & Hamburg, D.A. A psychoendocrine study of severe psychotic depressive crises. American Journal of Psychiatry, 1965, 122, 72-80.
Bunney, W.E., Jr., Mason, J.W., & Hamburg, D.A., Correlations between behavioral variables and urinary 17-Hydroxy-corticosteroids in depressed patients. Psychosomatic Medicine, 1965, 27, 299-308.
Cahill, G.F. Advances in enzyme regulations. Vol. 2. New York; Macmillian Company, 1964.
Connason, B.F., & Ryberg, R.A. Stress conditioning in schizophrenia and neurotic disorders, Diseases of the Nervous System. 1957, 18, 7.
Curtis, G. C., Cleghorn, R.A., & Sourkes, T.L. The relationship between affect and the excretion of adrenaline, noradrenaline, and 17-hydroxycorticosteroids. Journal of Psychosomatic Research, 1960, 4, 176-184.
Fajans, S.S. Unpublished Lecture.
Freud, S.A. General introduction to psychoanalysis (translated by Joan Riviere) Garden City New York; Garden City Publishing Co. 1943.
Graham, B.F., & R.A. Cleghorn, R.A. Changes in the circulating leukocytes following electrically induced convulsions in man. Journal of Clinical Endocrinology, 1951, 11, 1469.
Harvard Encyclopedia, 1891 Volume 23.
Hoffer, A., Osmond, H., Callbeck, M.J. & Kahan, I. Treatment of schizophrenia with nicotinic acid and nicotinamide. Journal of Clinical and Experimental Psychopathology, 1957, 18, 131-158.
Ingle, D.J. The chemistry and physiology of hormones. Washington, D.C.: American Association for the Advancement of Science, Smithsonian Institution, 1944.
Kaplan, M. Informal Communication.
Larsen, Virginia L. Physical characteristics of disturbed adolescents. Archives of General Psychiatry, 1964, 10, 55-64.
Long, C.N.H., Katzin, B. & Fry, E.G. The adrenal cortex and carbohydrate metabolism. Endocrinology, 1950, 26, 309.
Meyer, A. Commonsense psychiatry. New York: McGraw Hill, 1948.
Modern drug encyclopedia and therapeutic index, 1965.
New Drugs, Chicago, Illinois: American Medical Association, 1966.
Persky, H., Maroc, J., Conrad, E. & Den Breeijen, A. Blood corticotropin and adrenal weight-maintenance factor levels of anxious patients and normal subjects. Psychosomatic Medicine, 1959, 21, 379-386.
Plager, J.E. & Matsui, N. In vitro demonstration of the anti-insulin action of cortisol on glucose metabolism. Endocrinology, 1966, 78, 1154.
Portis, S.A. Life situation, emotions and hyperinsulinism. Journal of the American Medical Association 1950, 142, 1281.
Portis, S.A. & Zitman, I.H. Mechanism of fatigue in neuropsychiatric patients, Journal of the American Medical Association, 1943, 121, 569.
Physician's guidelines of diagnosis and treatment of hypoglycemia or the hypoadrenocortical state. The Hypoglycemia Foundation, Scarsdale, New York, 1966.
Roberts, H.J. The roles of diabetogenic hyperinsulinism in pathogenesis of prostatic hyperplasia and malignancy. Journal of the American Geriatrics Society, 1966, 14, 795.
Selye, H. The general adaptation syndrome and the diseases of adaptation. Journal of Clinical Endocrinology, 1946, 6, 117.
Simon, G.B. & Gillies, S.M. Some physical characteristics of a group of psychotic children. British Journal of Psychiatry, 1964, 110, 104-107.
Simpson, G.M. Drug therapy in mental illness. Effective participation by general practitioners. Postgraduate Medicine, 1966, 39, 557.
Suwa, N., Yamashita, I., Owada, H., Shinohara, S., & Nakazawa, K. Psychic state and adrenocortical function: A psychophysiologic study of emotion. Journal of Nervous Mental Diseases, 1962, 134, 268-276.
Tintera, J.W. The hypoadrenocortical state and its management. New York State Journal of Medicine, 1955, 55, 1869.
Tintera, J.W., Stabilizing homeostasis in the recovered alcoholic through endocrine therapy: Evaluation of the hypoglycemic factor. Journal of the American Geriatrics Society, 1966, 14, 126.
Tintera, J.W. & Lovell, H.W. Endocrine treatment of alcoholism. Geriatrics, 1949, 4, 274.